Anxiety is a feeling of worry, nervousness, unease, and a cause of insomnia. The CES Ultra CES device helps to relieve the anxiety-insomnia cycle…


Anxiety is a feeling of worry, nervousness, unease, and a cause of insomnia. The CES Ultra CES device helps to relieve the anxiety-insomnia cycle…

The COVID-19 pandemic has had a direct effect on the anxiety levels of all of us. Those who suffer from the symptoms of anxiety can find their symptoms heightened further due to the added stresses of trying times. Anxiety produces long term stress. Long term stress...

Living through the uncertainties of the coronavirus pandemic is raising anxiety levels, especially among people sheltering in place. This is a new experience for people who do not suffer from anxiety disorders under normal circumstances. Their anxiety can act as an...

Vagus Nerve Stimulation Vagus nerve stimulation (VNS) is a medical treatment that is routinely used in the treatment of epilepsy and other neurological conditions. VNS studies are not just clinically, but also scientifically informative regarding the role of the vagus...

Chionophobia is defined as an intense fear of snow. As in most phobias, Chionophobia is driven by anxiety and categorized as a Natural Environment Phobia. According to a study carried out by the American Meteorological Society, Chionophobia is the second most...
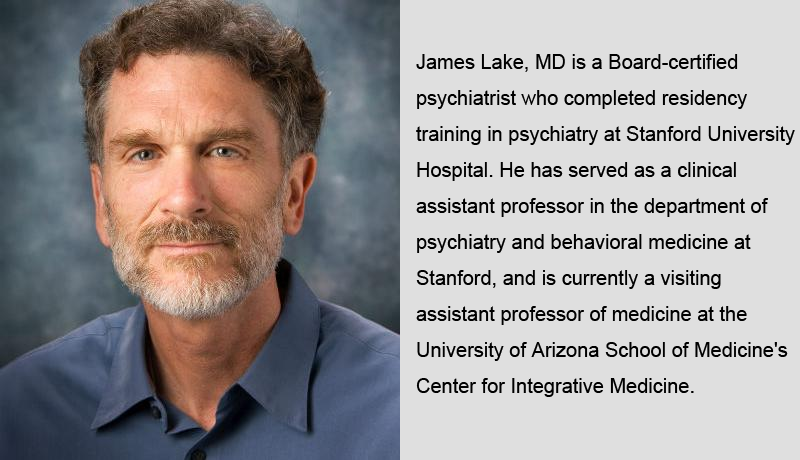
The growing use of anti-anxiety pills reminds some doctors of the early days of the opioid crisis. Considered relatively safe and non-addictive by the general public and many doctors, Xanax, Valium, Ativan and Klonopin have been prescribed to millions of Americans for...

Alternatives to Drugs in the Treatment of Depression It’s estimated that around 30 percent of people with depression don’t respond to typical antidepressants. This is known as treatment-resistant depression. An important alternative which can be life-changing is brain...
Cranial electrotherapy stimulation (CES) has beneficial effects on many mental problems Micro-current electrical stimulation, also called cranial electrotherapy stimulation (CES), has been approved by the U.S. Food and Drug Administration for treatment of insomnia,...

With the increasingly stressful lifestyle there is also rise in other types of disorders such as anxiety and sleep disorders. With the lack of sufficient treatments that address these disorders, cranial electrotherapy stimulation comes as an innovative and required...
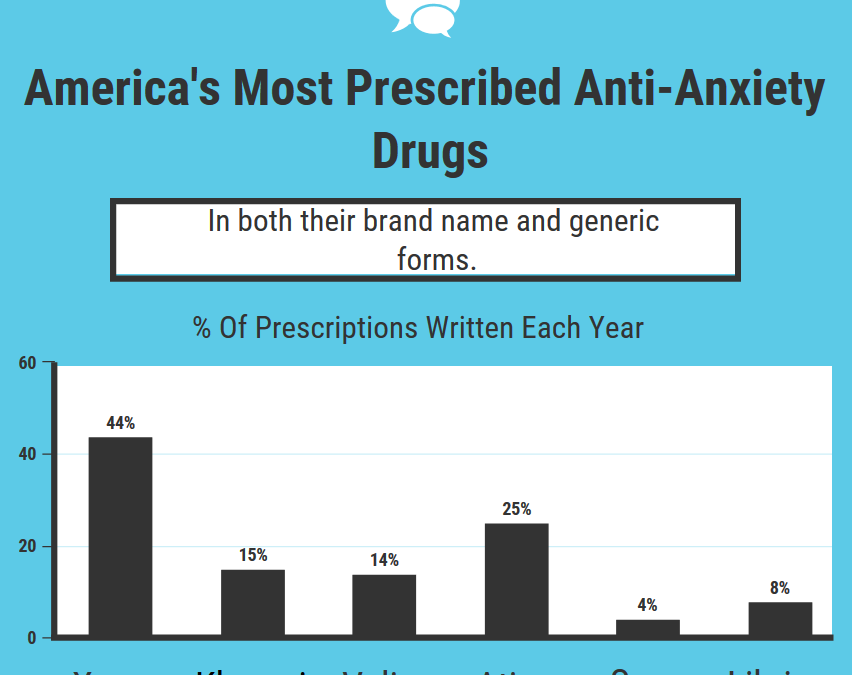
Anxiety disorders are the most common mental illness in the U.S., affecting 40 million adults in the United States age 18 and older, or 18.1% of the population every year. Considered relatively safe and non-addictive by consumers and many doctors, Xanax, Valium,...