Anxiety, CES Ultra device, Insomnia, PTSD
Living through the uncertainties of the coronavirus pandemic is raising anxiety levels, especially among people sheltering in place. This is a new experience for people who do not suffer from anxiety disorders under normal circumstances. Their anxiety can act as an...

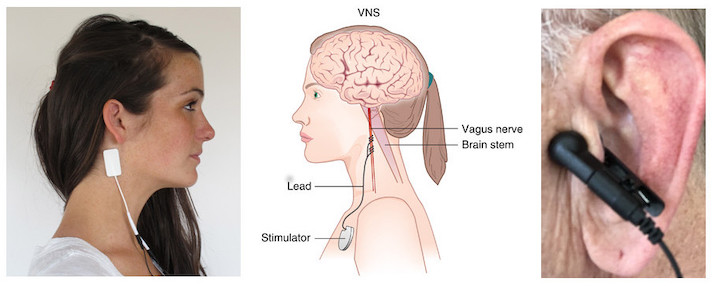
Anxiety, Inflammation, Sadness, Vagus Nerve Stimulation
Vagus Nerve Stimulation Vagus nerve stimulation (VNS) is a medical treatment that is routinely used in the treatment of epilepsy and other neurological conditions. VNS studies are not just clinically, but also scientifically informative regarding the role of the vagus...

Anxiety, CES Ultra device, Sadness
Chionophobia is defined as an intense fear of snow. As in most phobias, Chionophobia is driven by anxiety and categorized as a Natural Environment Phobia. According to a study carried out by the American Meteorological Society, Chionophobia is the second most...

CES Ultra device, Inflammation, Vagus Nerve Stimulation
Note: The CES Ultra does not make claims as to alleviation of pain. However this article shows how inflammation and symptoms of arthritis may be reduced by Vagus nerve stimulation. The CES Ultra targets the Vagus nerve. Inflammatory responses play a central role in...

Alternative Health, Anxiety, Insomnia, Sadness
Focus Factor® bottle, not equal to symbol, fresh fruits, vegetables and nuts Focus Factor is a memory booster that provides supplemental nutrition to help you feel sharper and more alert. The ingredients of Focus Factor are vitamin A, vitamin C, vitamin D, vitamin E,...